Severe eye pain
Blurry vision
Eye injury
At Balaji Eye Care Hospital, Dr. Jayadatt Patel, a fellowship-trained cornea and ocular surface surgeon, offers expert treatment for keratoconus, corneal infections, dystrophies, and dry eye disorders using advanced techniques.
When it comes to cornea care, you deserve nothing but the best. At Balaji Eye Care Hospital, we are proud to have a team of highly skilled and experienced corneal surgery experts. Dr Jayadatt Patel ranks top among the best cornea specialists in Ahmedabad. We are dedicated to providing you with comprehensive and personalized corneal treatment.



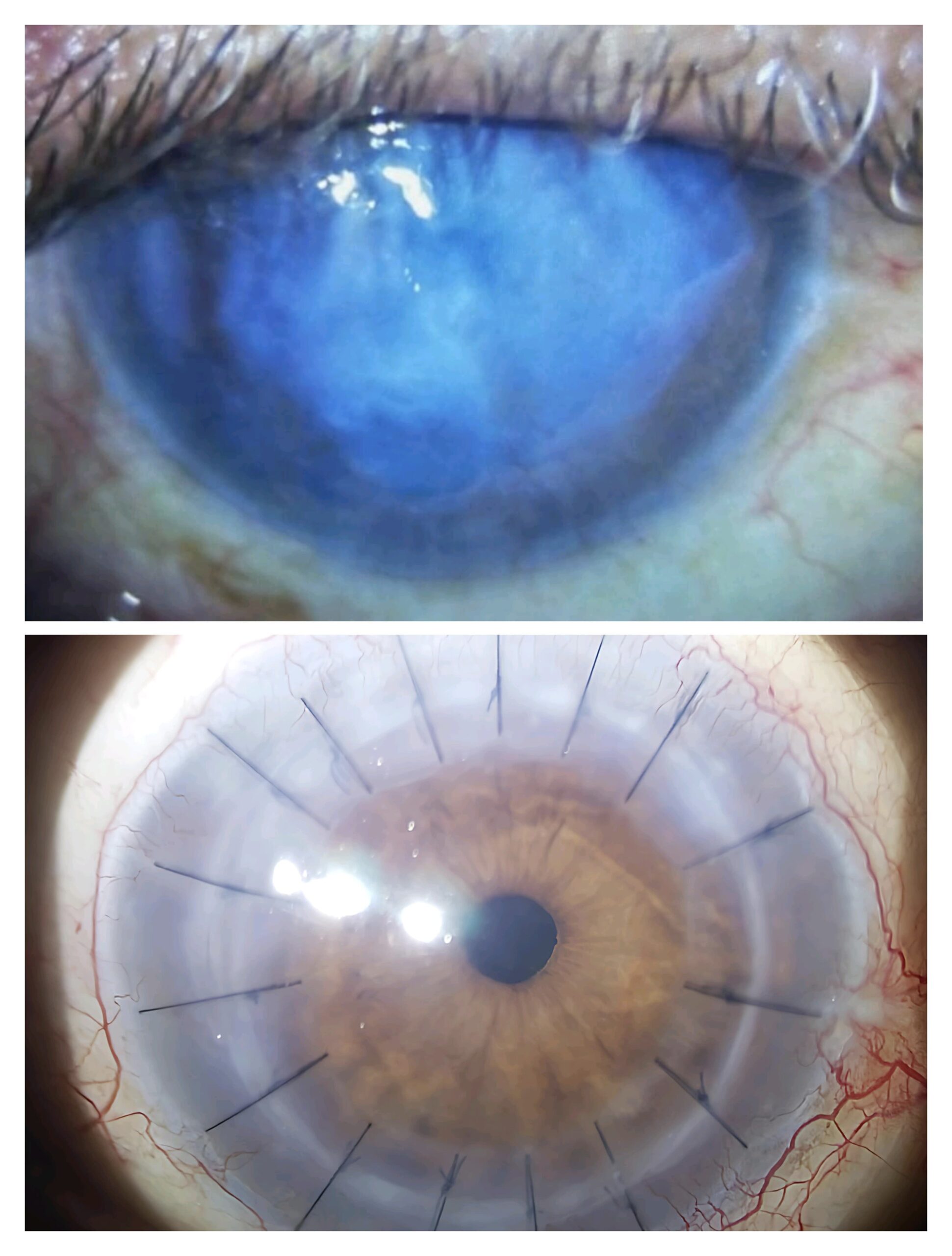
Keratoconus weakens and bulges the cornea, producing blurred vision and light sensitivity. It begins at adolescence and progresses. Mild cases are treated with lenses, and severe cases are operated on. Reasons are genetics, eye rubbing, and tissue issues.
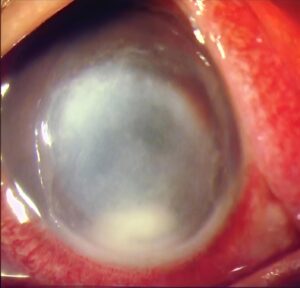
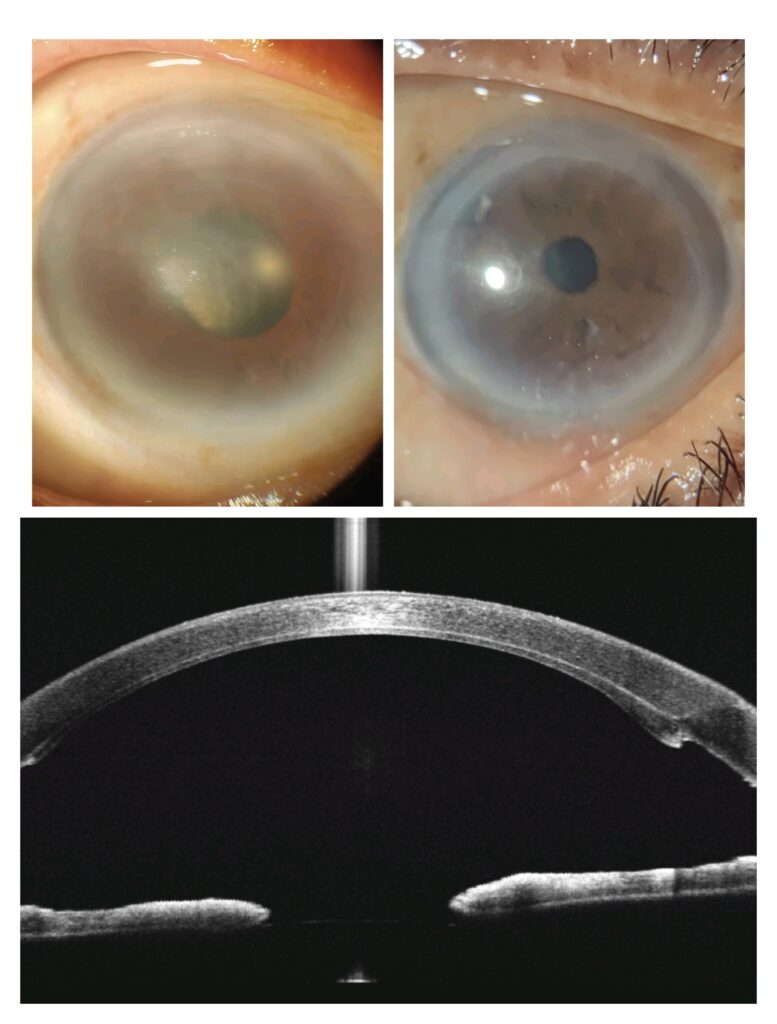
Bullous Keratopathy leads to corneal edema and painful blisters from injured endothelial cells. It may be caused by surgery, trauma, or diseases such as Fuch's Dystrophy. Its treatments are medication, special glasses, or corneal transplantation in extreme situations.
Genetic mutations cause inherited corneal diseases such as granular, lattice, and macular dystrophy, resulting in protein deposits, impaired vision, and pain. The symptoms begin during early adulthood and progress with time. Medications, lenses, or corneal transplants are the treatment options.
Scars on the cornea are caused by injury, infection, or surgery that hurts the smooth surface of the cornea, causing blurred or distorted vision. Based on the severity, medications such as medicated eye drops or laser treatment can minimize scarring and enhance clarity.
Contact us immediately if you experience:

Many corneal conditions can be effectively managed with prescription eye drops or oral medications. These treatments help reduce inflammation, fight infections, and promote healing of the corneal tissue.
If corneal damage cannot be repaired, a transplant may be necessary. This involves replacing the damaged cornea with healthy donor tissue. For more details, book a consultation.

In cases of certain corneal dystrophies and related conditions, employing a laser-based procedure known as phototherapeutic keratectomy (PTK). PTK is used to reshape the cornea, eliminate scar tissue, and improve visual clarity.
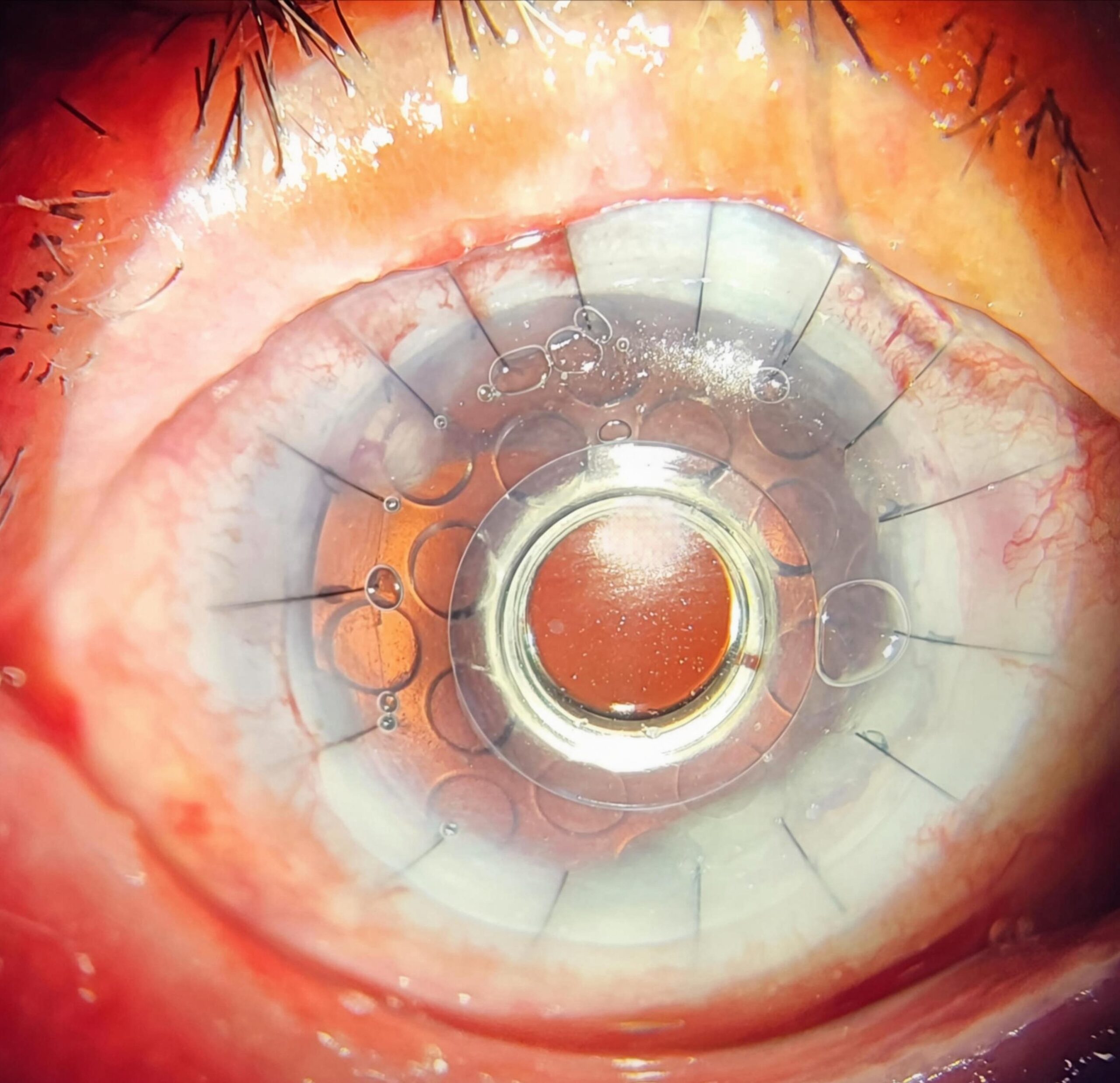
As an alternative to traditional corneal transplant surgery, some patients with damaged corneas may receive an artificial cornea, known as a keratoprosthesis (KPro).
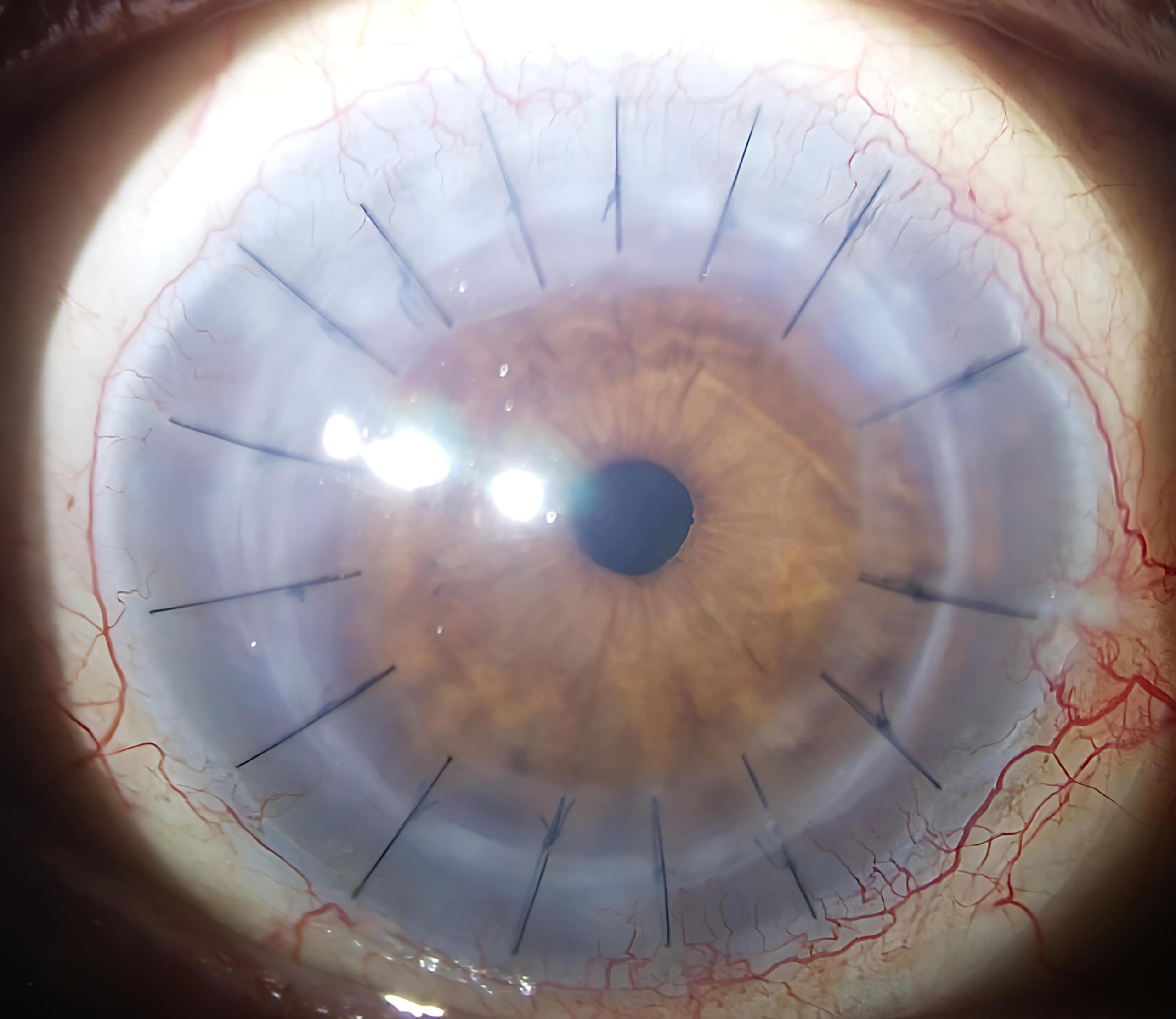
Penetrating Keratoplasty replaces the entire corneal thickness with healthy donor tissue, restoring vision in severe cases of corneal scarring or disease. It is commonly used for advanced corneal conditions.
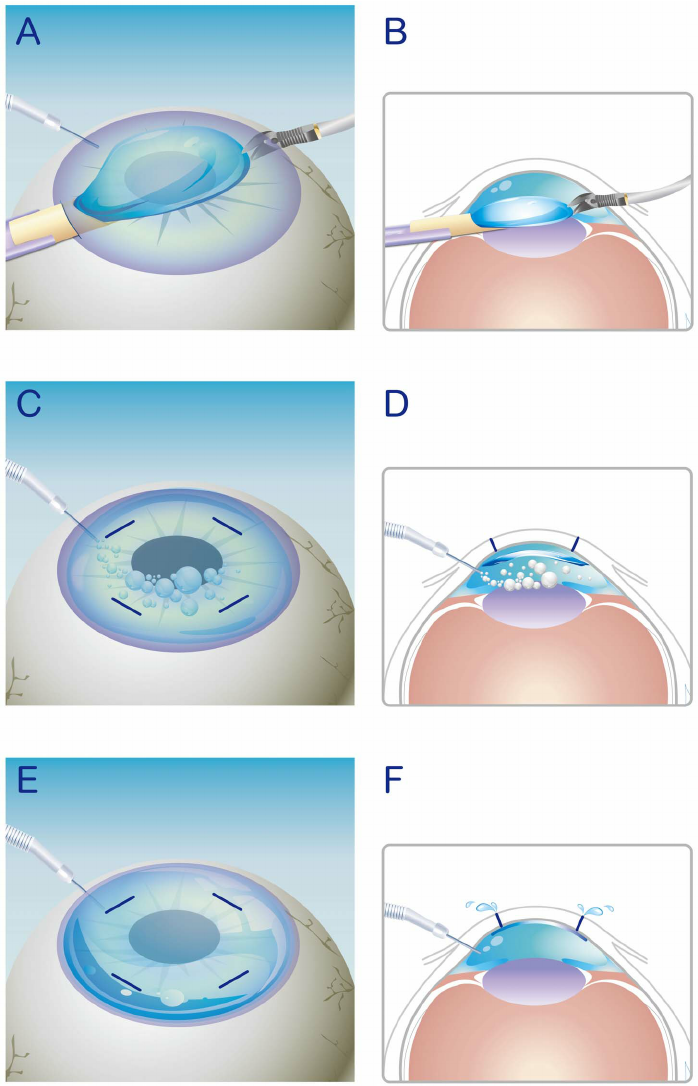
Lamellar Keratoplasty substitutes damaged corneal layers only and therefore preserves healthy tissue. It diminishes the chances of graft rejection while increasing the rate of healing relative to full-thickness transplants.
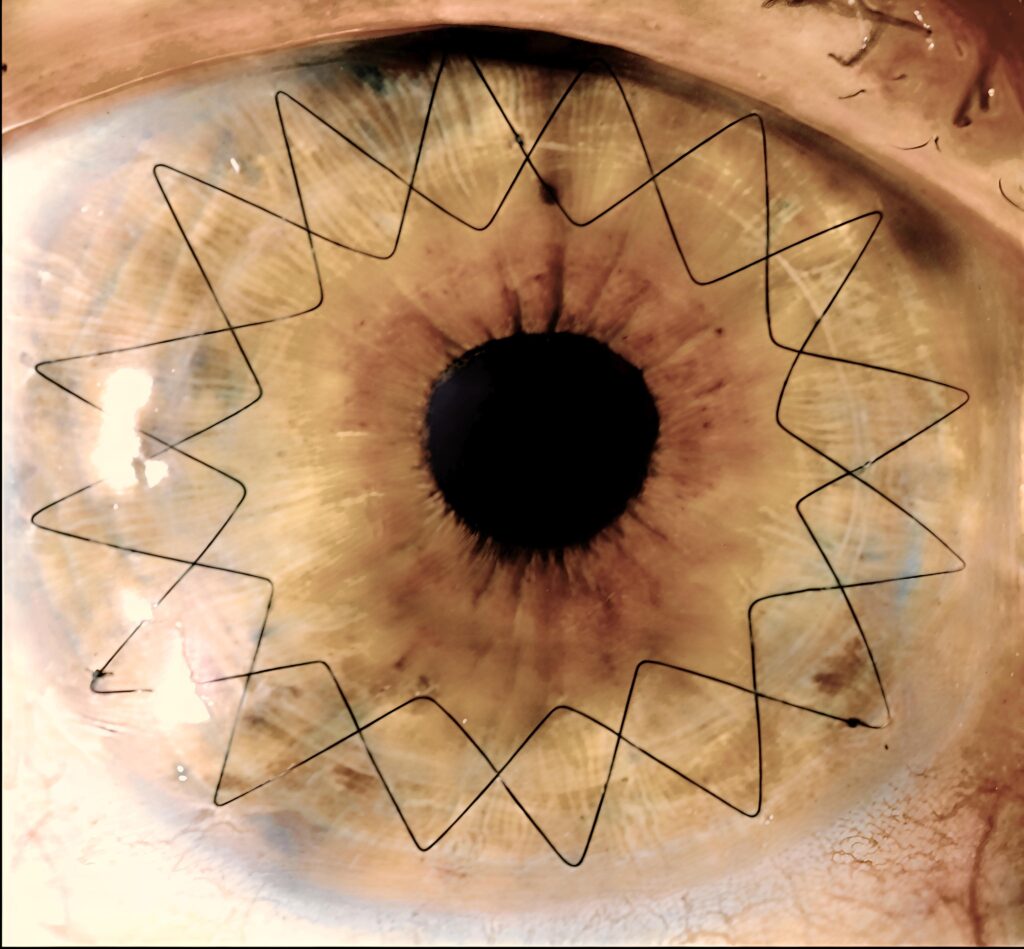
This includes several subtypes where only a portion of the cornea is replaced:
In DALK, the anterior portion of the cornea with the endothelial layer is replaced, which substantially decreases rejection chances and improves the rate of post-operative healing.
The SALK method is indicated for superficial corneal injury; it replaces only the most superficial corneal tissues. As the cornea’s deeper parts are preserved, it helps avoid complications and ensures faster healing.
This includes several subtypes where only a portion of the cornea is replaced:
The Inner layer of the cornea with the endothelial layer and Descemet’s Membrane is replaced with outer layers intact in DSAEK. The use of these techniques routinely gives quicker convalescence and leads to fewer complications than full-thickness transplants.
Only the diseased Descemet’s membrane and endothelial cells are removed in DMEK, which provides the best vision due to the least obstructions with the most rapid recovery period offered, requiring the best surgical skill.
Recovery varies greatly depending on the individual and the type of transplant. Full visual recovery can take several months or even years.
Most corneal transplants are successful in improving vision and quality of life. Long-term success depends on proper post-operative care and adherence to medication regimens.
Requires careful eye drop medications to prevent infection and rejection. Vision may improve gradually over several months or years. Regular follow-up appointments with the ophthalmologist are essential.
It may be possible in some cases, but depends on the type of transplant and the healing process.
Yes, long-term medications to prevent rejection are usually required.
Discomfort is common after surgery, but usually well-controlled with pain medication.
Rejection: The body may reject the donor cornea.
Infection: Risk of infection during or after surgery.
Glaucoma: Increased pressure within the eye.
Cataracts: Clouding of the eye lens.
Astigmatism: Irregular curvature of the cornea.
If you’re seeking the best cornea specialist doctor or considering a cornea transplant in Ahmedabad, look no further. Balaji Eye Care is one of the best cornea care hospitals in Gujarat.
Science City
Opening Hours
Monday-Saturday
Sunday-only appointments
Copyright © 2024 balajihorizoneyecare.com . All Rights Reserved.
Designed by EEG Technogeeks.